The following are some things we learned concerning self funded health care plans. We learned these lessons the hard way, and hope to help others before they would ever be in the position we were in with our sweet ME.
We are not lawyers, just a family who learned from their hard and painful experience.
**Please contact
Employee Benefits Security Administration
(ERISA 1-866-487-2365)
and/or a lawyer to confirm these lessons.
1. Get a copy of the plan from your HR. The real plan. If your company is fully funded it won’t be branded by a third party health care logo.
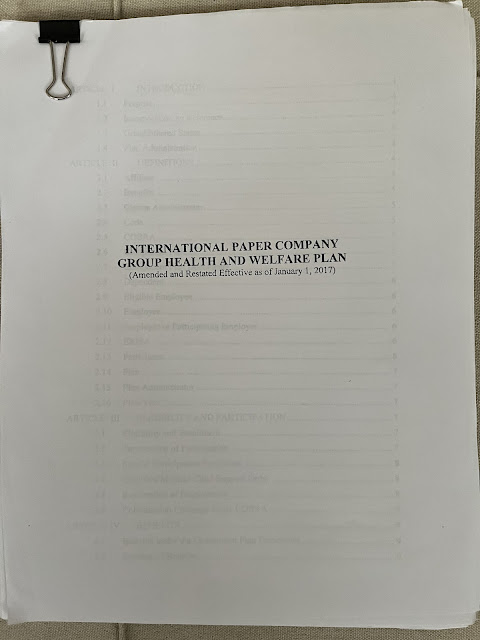
This first one is not “the plan”. Cigna is not our actual plan. They just help administer it.
These next two photos show the actual plan. They are very important to request. The SPD and the actual plan should both be sent to you, free of charge, and promptly.
Read the plan carefully, and get guidance from your doctor and medical team. If it’s in the plan, the treatment is covered and required by ERISA and good faith laws to be approved.
2. Follow the appeal process and document, document, document. If they call to discuss, or stop you in the hall, ask them to email you what ever they want to discuss. Even if you know the individual well.
3. Consult a lawyer if you want, but don’t retain one. It is one of the first questions you’ll be asked when you contact EBSA, (ERISA 1-866-487-2365) and the EBSA investigators will inform you that they can’t work with you if you did. After they’ve helped you, you can retain a lawyer if you’d like.
4. Declare whistleblower protection if you are afraid of retribution.
5. If they aren’t following their actual plan, call EBSA (ERISA 1-866-487-2365) do what the EBSA investigator says.
6. Things to watch out for:
~Watch out for a self funded health care plan giving a denial because your prescription is not FDA approved. Up to 40-60% of drugs are administered through the off-label process. Your doctor will know if your medicine falls under off-label. Your doctor also knows the off label process, and should be prepared to do it.
~If you have more than one insurance plan, some companies will deny and run you through a series of appeals, and then your secondary picks up the claim. This is an indicator that something is wrong. This is a red flag, and you should contact EBSA and your secondary insurance to report this.
-For those of you who like speaking to managers when something seems wrong, speaking to your third party administrator’s top manager is not effective, unless it’s a simple paperwork problem. In our case, the SVP of Human Resources is the actual plan administrator. That position has the final say. The person who has this role is listed in the actual plan, and that person is required to follow the plan in good faith.
If you are concerned about any or all of the above or it has happened to you, you can still report, and likely still appeal. Simply call EBSA (ERISA 1-866-487-2365).
All of this to say, the determination process should be done in good faith, smoothly and promptly.
Ask for help by EBSA (ERISA 1-866-487-2365) if this is not the case. They will walk you through the process of determining what you need to say to your health care administrators as you request that they follow the plan in good faith.
EBSA investigators are willing to talk to your Health Care Plan administrators as well, to help guide them.
Though, truthfully, if they (your health care administrators) don’t know all of this, that’s concerning, and a red flag, and worth reporting to EBSA (ERISA 1-866-487-2365)
We hope any of what we’ve been through will help you be your best as an advocate for you or your family member.
*PS our story is not over. We will keep updating here.
John has offered to be able to use what happened to us as a lesson to his colleagues on what to do if you’re in a similar situation. The company calls it LIFE Lessons. He recommended this on a Help Line call claim on December 19, 2022. He is still awaiting an answer.